The health care sector can increase access to healthy foods while addressing the social and environmental determinants of health in their communities, by creating jobs and contributing to a strong and equitable food economy.
Invest in healthy people, places, and economies
Local food has become a priority for individuals and institutions across the country. From 2006 to 2014 the number of farmers markets increased by 180%, sales to food hubs (local food aggregators) increased by 288%, and farm-to-school programs increased by 430%. Local food sales in the United States were estimated to be $8.7 billion in 2015.
Over the past 50 years, food and agribusiness companies have prioritized efficiency in food production, processing, storage, and distribution. Diversified farms growing multiple food items have given way to specialization, and fewer and fewer companies are producing, processing, and distributing our food. This consolidation is also seen geographically, with particular states or regions producing the bulk of what we eat, and other states and regions producing very little.
The consolidation of the food system has led to:
- The economic decline of rural communities
- Fewer opportunities for farmers and food companies that are small and mid-sized and owned by people of color
- A general lack of control and connection to food production
- Environmental degradation
Defining local
Health Care Without Harm and Practice Greenheath define “local" as food grown/raised/ harvested/ processed within 250 miles of the health care facility (500 miles for meat, poultry, and seafood).
Compounding this trend, diet-related diseases have become the leading causes of death in the United States, disproportionately impacting low-income and communities and people of color. While we produce an abundance of food, a great deal of it is highly processed which is counter to dietary guidance from the Department of Agriculture and contributes to poor health outcomes.
Rebuilding local and regional food systems can address these interrelated, complex issues by giving communities greater control over food production, providing jobs and opportunities, and increasing access to healthy, fresh foods.
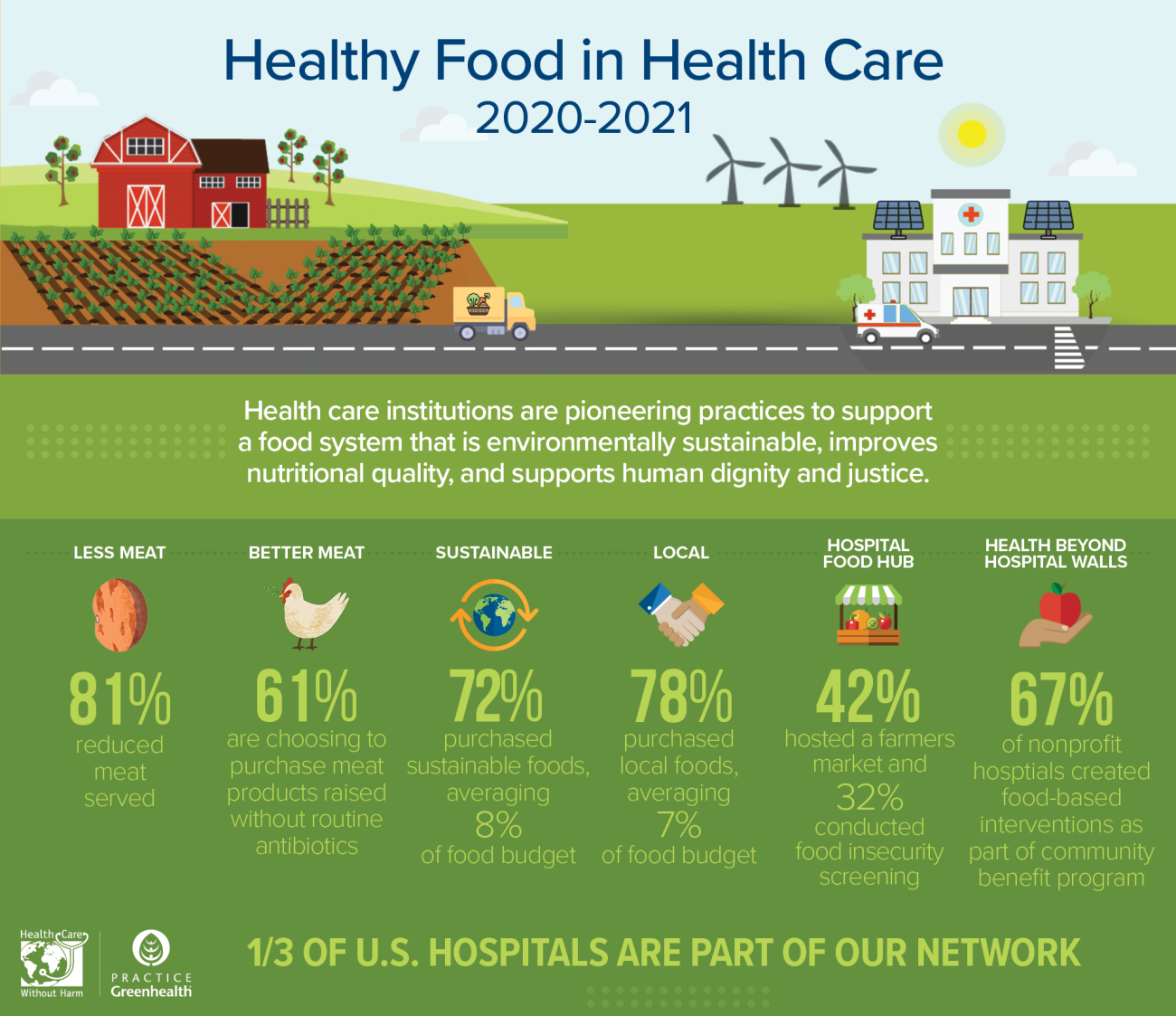
In 2021, Health Care Without Harm and Practice Greenhealth found that 78% of health care survey respondents spent, on average, 7% of their budgets on local foods, using a variety of supply chain pathways.
Employee and patient health and satisfaction
1) Improves nutrition and taste
“With just 1 in 10 adults meeting the federal fruit or vegetable recommendations, better tasting fruits and vegetables can encourage increased consumption, thereby reducing the risk of many leading causes of illness and death, including heart disease, type 2 diabetes, some cancers, and obesity.”
— Centers for Disease Control and Prevention
Produce picked at peak ripeness tastes better and may be more nutritious. Food that is harvested in anticipation of a long transport is often picked underripe, reducing its nutritional value and compromising taste.
The longer a food spends off the vine, the greater the loss of vitamins, minerals, and other nutrients.
- One study showed nutrient losses from 15% for green peas to 77% for green beans when stored at 39 degrees for 7 days.
- Another study found that the nutrient content of broccoli was cut in half when it was purchased out-of-season from national markets, compared to when it was sourced locally while in season.
Foods consumed in the United States can spend anywhere from two days to multiple weeks in transport depending on the point of origin.
In a local food system, the supply chain and distance traveled is shortened, which enables foods to be picked riper and consumed closer to harvest. This provides the consumer with better tasting foods at their peak of nutritional value.
2) Improves patient and employee satisfaction
People are increasingly interested in knowing where their food comes from and prefer local foods. Surveys show 87% of grocery shoppers say the availability of local food is either “very” or “somewhat” important in choosing a primary grocery store, and two-thirds of respondents said they choose a restaurant based on local food options.
Consistently listed as a “hot trend” by the American Restaurant Association and as health care food service trend, this preference is not limited to “high-end” establishments but is reported among casual, fast-casual, and quick-service dining as well.
This broad interest across food establishments demonstrates that local food is not a priority of a select group, but relevant to the population at large. Further, many report that when given a choice, they would select menu items featuring local ingredients at a slight price premium.
This preference for local foods is reflected in Press Ganey score improvements among hospitals that have increased their service and marketing of local foods.
- In 2006, New Milford Hospital in Connecticut was in the 30th percentile nationally for their food service. After their dining services started to highlight local, fresh foods, the hospital’s scores shot up to the high nineties.
- Cottage Health in California experienced a similar score increase when they began using organic, local ingredients. They went from a Press Ganey ranking of 43% to 83% for their meals.
- Hospital Consumer Assessment of Healthcare Providers and Systems scores, which are factored into Medicaid and Medicare reimbursements, can also be improved by a patient’s food experience.
Cooking with fresh, local ingredients also improves food service employee satisfaction due to the skills they learn and the sense of fulfillment they gain from serving food aligned with the hospital's mission. For employees at Mercy Medical in Iowa, allocating the extra labor required to cook with fresh ingredients was challenging at first, but after seeing the reaction from the individuals they served, employees felt “proud of what they were producing.”
Addressing the root causes of health
3) Creates community wealth and jobs
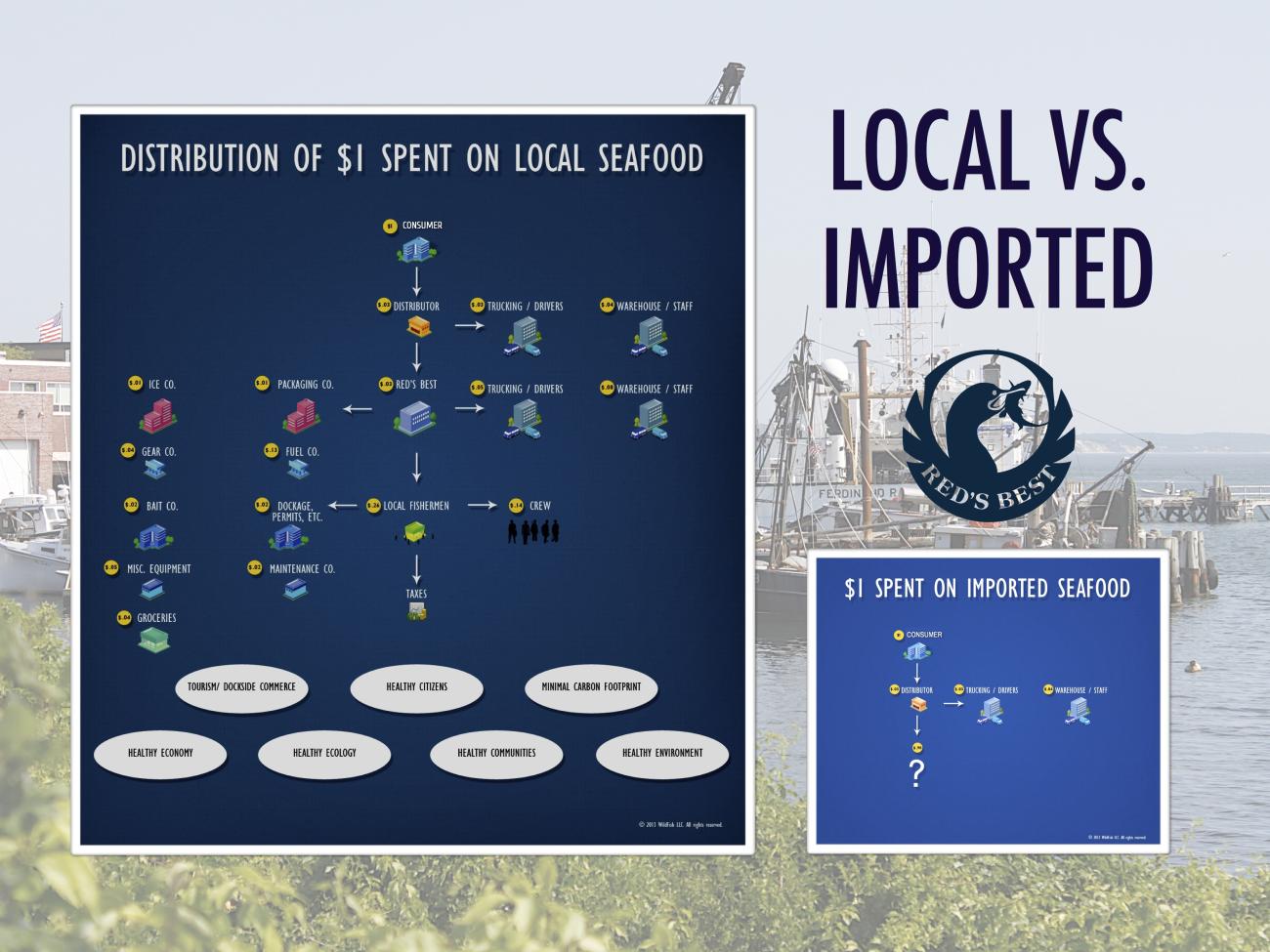
The USDA reports that every $1 million spent on local foods supports 13 on-farm jobs.
Social factors, including education, income, and poverty, accounted for over a third of total deaths in the United States in a year. When hospitals buy local they address these social and environmental determinants of health by creating jobs and building community wealth.
In addition to jobs in agriculture, buying local supports related businesses like processors, aggregators, distributors, cold-storage facilities, and equipment manufacturers – all of which provide additional jobs. A review of five different foods sold locally versus the national market found that farmers earned 50 to 649% more for their products due to a shortened supply chain and that nearly all of the wage and proprietor income remained in the local economy.
Examples from Georgia and Ohio illustrate the power of local foods in community development.
- Researchers found that if Georgia residents spent just $10 of their weekly food budget on local foods, it would generate $2 million in sales revenue for the state’s producers.
- A study of agriculture in northeastern Ohio found that if farmers met just 25% of the demand for food in their region, 27,664 new jobs would be created, providing work to about one in eight unemployed residents, and annual regional sales would rise by $4.2 billion.
Hospital investment in local food pays off
The University of Vermont’s Center for Rural Development examined the effect of the University of Vermont Medical Center’s local purchasing on the economy. In 2012, the Practice Greenhealth member hospital spent $1.78 million on local food, resulting in a total economic output ranging between $3.53 million and $4.71 million, creating 24 to 30 jobs. The hospital’s purchasing had an economic multiplier ranging from 1.98 to 2.64, meaning that for every dollar spent on local food by the hospital an additional $0.98-1.64 was added to the local economy.
4) Creates equitable communities and addresses food insecurity
When hospitals invest in local food systems they can provide opportunities for populations that have historically been excluded, and subsequently address the social and environmental determinants of health.
The federal Office of Disease Prevention and Health Promotion Healthy People 2020 framework states that health disparities adversely affect groups of people with “characteristics historically linked to discrimination or exclusion” such as racial or ethnic group, religion, and socioeconomic status. These populations also experience disproportionately high rates of food insecurity, lower incomes, lack of social capital, and lack of land and home ownership.
In two separate reports, the USDA and the St. Louis Federal Reserve Bank both found that investment in local food systems can combat structural inequalities and increase food equity. Many organizations addressing food inequity are looking beyond the charitable feeding model and are utilizing local food markets to provide job training and education and to develop pathways for underserved communities to build and acquire capital resources.
Local food markets can be easier to access in comparison to national or international markets which require greater capital investment. When health care invests in local food systems they can provide opportunities for populations that have historically been excluded, and subsequently address the social and environmental determinants of health.
Increasing equity through employment
Boston Children’s Hospital, a Practice Greenhealth member, supports communities through their purchasing relationship with CommonWealth Kitchen, a community development corporation based in Boston. CommonWealth provides kitchen space to over 50 food businesses, 75% of which are owned by women and immigrants, many of whom are people of color, who employ nearly 150 people in one of Boston's lowest-income neighborhoods. Each year, three to five of these companies "graduate" into their own dedicated retail or production space. Since their inception in 2009, CommonWealth has "graduated" over 50 companies that are still in business today, creating more than 500 jobs.
Community resiliency
5) Protects farmland and the environment
According to American Farmland Trust, over 40 acres of farmland are lost each hour in the United States due to urban sprawl. Further, 91% of fruits and 77% of vegetables are grown on “urban edge” farms that are under threat of development. Pressure to develop farmland is strong as property values rise, particularly lands in relatively close proximity to metropolitan areas, because development brings higher revenues than farming.
However, well-managed farmland provides services to the community that are not captured in an analysis based solely on revenue from the land.
Farm’s using ecologically sustainable practices also perform ecosystem services:
- preserving and building topsoil which absorbs carbon from the atmosphere
- protecting water sources
- maintaining open spaces like fields, forests, and meadows
- preserving genetic diversity
Farms growing for local markets often maintain genetic diversity because they grow a wider variety of crops than farms growing for national markets, which grow for standardization and a long route to the plate.
Maintaining farmland also keeps taxes lower because farms generate more public revenue than they receive in public services, whereas residential use requires far greater public services.
Health care can help preserve farmland and maintain the services farms provide by buying food produced sustainably, locally and regionally.
Farms protect clean drinking water
New York City recognizes the role of sustainably managed farms in protecting water resources for its residents. The Watershed Agricultural Council works with farmers and foresters to implement environmentally sustainable practices and to conserve working lands in order to provide clean drinking water to more than 9.5 million New Yorkers every day. Since its inception in 2001, the council’s Agricultural Conservation Easement program has protected 25,845 acres of farmland in the watersheds that surround New York City’s reservoirs in the Catskills.
6) Ensures dependable food supply
The supply chains to population centers are getting longer with fewer goods and fuel on hand locally, leaving hospitals and communities vulnerable to interruptions during natural disasters, bacterial outbreaks, and other emergencies.
In successful regionally based food systems of the past, food was grown in surrounding rural areas and processed and warehoused in cities. Cities often had weeks of food on hand.
While the move toward consolidation in the food system has lowered prices and increased profits for food companies, it has made our system more vulnerable to events such as a bacterial outbreak, livestock or poultry disease, and extreme weather events.
- In 2013, Superstorm Sandy flooded New York City grocery stores, and road closures left some stores without food for two weeks.
- Flooding in Houston in 2017 left Ben Taub Hospital, the city's largest Level 1 trauma center, running critically low on food for days.
Natural disasters are expected to continue to disrupt our food system. Compounding this vulnerability, major food distributors and fuel suppliers have moved toward “leaner supply chains,” with oil refinery closures and food storage warehouses stocking less food to increase profitability.
A 2017 Johns Hopkins Center for a Livable Future report on the City of Baltimore’s food system resilience found that the geographic concentration of food processing and food distribution/warehouses, and the specialization in crop production could compromise their ability to access food in a crisis. The report recommended balancing their reliance on national and global food markets with local and regional food systems.
Health care can play an important role in building food system diversity and resiliency and ensuring a reliable food supply for their communities by supporting local and regional food producers.
Take action
By purchasing regionally grown foods from sustainably managed farms, health care has access to a wider variety of tastier, fresh foods that can be enjoyed seasonally and at their peak of nutritional value.
Buying regional foods can also contribute to community development, providing jobs and opportunity for disadvantaged communities, and can support the local economy, building community wealth.
Health care can take action now to provide healthier food to patients and staff, while preserving farmland, protecting our environment, and ensuring a reliable food supply.
- Refer to the Healthy Food in Health Care standards and guidance resources for additional strategies and resources to support planning, implementing, and tracking the impact of your local food purchasing efforts. Join Practice Greenhealth for more information and assistance in meeting your food goals, individualized technical assistance, and national recognition for your work in supporting the local food system.
- Communicate with your vendors about your preference for locally and regionally produced foods. Health Care Without Harm and Practice Greenhealth define local as food grown/raised/ harvested/processed within 250 miles of the health care facility (500 miles for meat, poultry, and seafood) and assists the sector in strategies to increase purchasing. Ask your vendors to help you identify local foods by listing source of origin so you can track and share your progress.
- Utilize RFPs and contracts with vendors to ensure they will help you meet your goals in sourcing local foods. Farm to Institution New England’s Food Service Toolkit provides guidance and sample RFP and contract language.
- Buy direct from a farm or seek out food hubs, co-ops, or other distributors that specialize in local foods. Contract with a farmer and engage in pre-season planning so they can grow according to your needs.
- Employ culinary strategies such as seasonal menus that make use of the freshest food in your region. Local foods that are in season can be price competitive with foods sold nationally. Reducing meat on your menu is another cost-saving culinary strategy, which can result in savings that can be funneled to local produce and sustainably raised local meat.
- Buy underutilized produce and seafood. Farm seconds, also known as “ugly fruit,” which may not be suitable for retail markets because of their appearance, are perfect for institutional kitchens. Ask local farmers or distributors about seconds in order to save money and prevent food waste. Many of the seafood species in our local waters are underutilized because they are unfamiliar, yet make excellent substitutes for more commonly known fish. Our seafood guide can help you prioritize local, wild seafood.
- Make community benefit investments in local food systems, which can improve access to healthy foods, address the social and environmental determinants of health, and create jobs. Visit our Delivering community benefit: Healthy food playbook to learn how health care facilities are increasing healthy food access and local food system growth through community benefit investment.